Gonioscopy
Gonioscopy may be the most challenging slit lamp exam skill to master, but learning to gonio is like getting scuba certified. You gain a lifelong skill to unlock a whole world! Except this is a world within the eye that can give you the key to the diagnosis and treatment of glaucoma, which might be almost as cool. Here are some tips to make it easy:
Set your patient up for success
Position patient well to allow full excursion of light beam (line up lateral canthus with mark on side bar, ensure patient can comfortably keep forehead touching the band)
Do other parts of the SLE including applanation prior to gonio (indentation gonioscopy may lower IOP)
Ensure ocular surface is sufficiently numb
Use careful wording “This lens comes close and you may feel it tickle your lids and lashes, please open both eyes wide and look straight ahead.”
Set yourself up for success
Turn off the room lights
Choose your favorite gonio lens (The Zeiss-style four-mirror or six-mirror lens is recommended for indentation gonioscopy)
Support your elbow on the slit lamp (use an elbow pad if needed)
Hold the lens with thumb and index finger, and use third and fourth fingers to help gently keep lids open
Use very gentle contact. If you intermittently briefly lose contact with the tear film, you are doing it correctly. If you see any corneal striae, you are using too much pressure and may open/distort the angle or inadvertently debride the corneal epithelium.
Use a medium-low intensity light beam at <50% height to avoid directly shining in pupil inducing constriction. Vary the width of the light beam to help grade the angle.
Start with the eye that has poorer vision, if able
Start with the superior mirror (inferior angle is usually deeper, more pigmented, and easiest to see) and scroll down to see other angles
And ultimately, practice makes perfect. Gonio the wide open normal eyes first. Knowing normal anatomy will help you appreciate pathology.
Please see these helpful videos for gonioscopy exam tips, courtesy of Dr. Lee Alward.
How do you describe the angle?
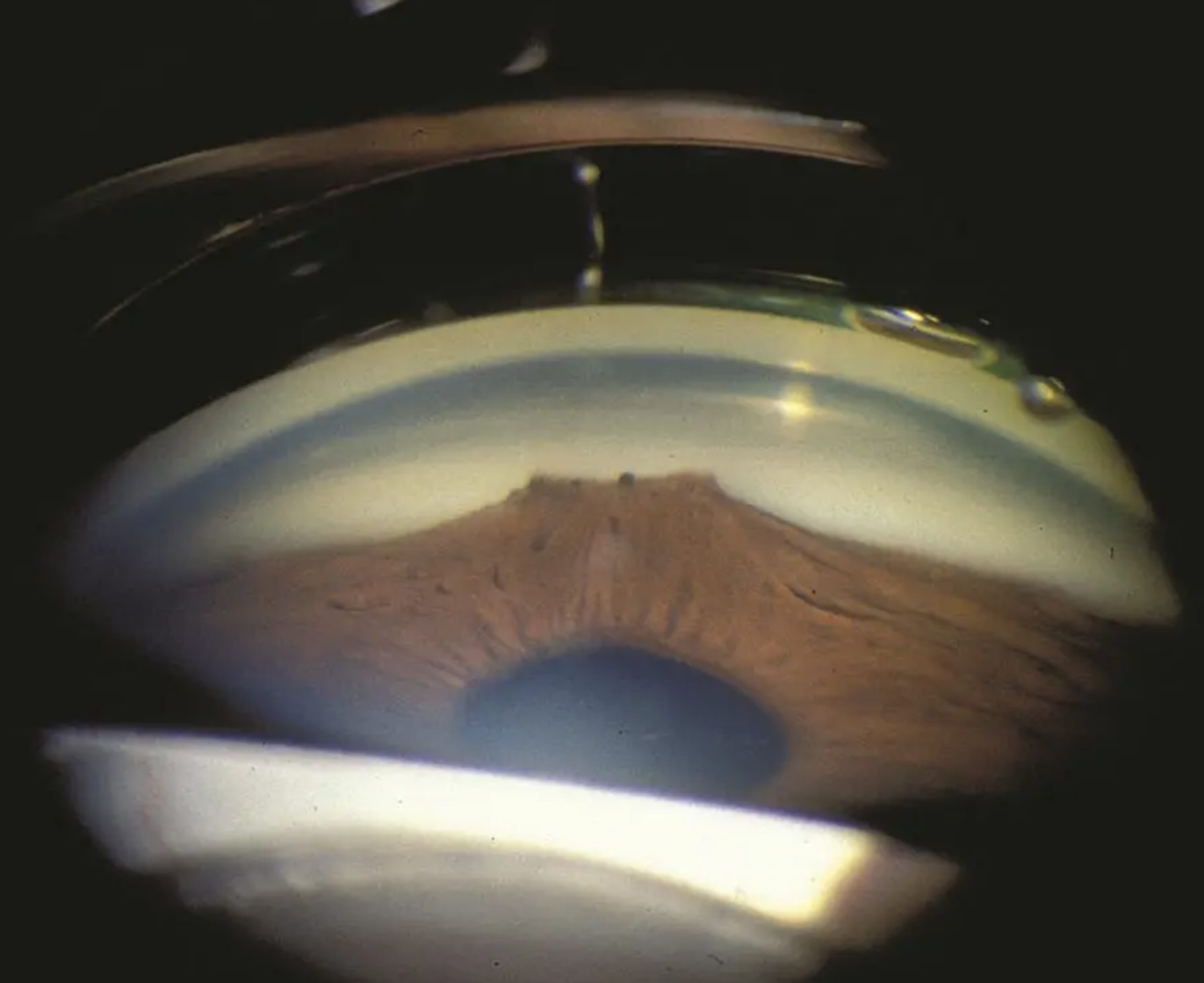
First step: determine if you can see structures. Here’s a mnemonic, from posterior to anterior:
I Can’t See This Sh…tuff.
Iris, Ciliary body, Scleral spur, Trabecular meshwork, Schwalbe’s line
But how do you describe what you are seeing?
There are many ways to describe the angle. The simplest way: open, narrow, closed, hyper-deep.
Another way is to simply describe what you can see, for instance:
Open to ciliary body band 360, light pigmentation
Open to scleral spur 270, to TM superiorly, heavy pigmentation
Open to scleral spur 360, patchy pigmentation, +sampaolesi line
Narrow, scattered PAS, areas of NVA
Angle recession from 3 to 8 o’clock
Another way is the Spaeth gonio grading system. A ton of info is crammed into a neat abbreviation, including information regarding iris configuration and indentation gonioscopy. It is easy as ABC:
A (no indentation)revealed with indentation
B angle degrees
C iris morphology
Examples:
A10b = closed
(A)B20b = at risk for closure
(C)D40f = open
E50c = angle recession
The angle grading is specified for each quadrant of the angle (superior, inferior, temporal, nasal). Even if you do not adopt the Spaeth gonio grading system, it is good practice to consider what structures you can see, the angle of iris insertion, and the iris configuration during gonioscopy. Each aspect contributes valuable information to your diagnosis and treatment considerations.
Here is an excellent library of gonioscopy videos showcasing a variety of neat exam findings for various diagnoses.